Malaria
Malaria is an infectious disease caused by the protozoan parasite of the Plasmodiumgenus. In 2020 alone, the disease caused an estimated 241 million cases and 627,000 deaths worldwide. Africa is the continent with the highest risk of malaria, accounting for 92% of infections and 93% of deaths recorded in 2017 (WHO).
CAUSES
The disease is caused by various types of single-celled parasites of the genus:
- P. falciparum: endemic in sub-Saharan Africa, Asia, Latin America, and the eastern Pacific
- P. vivax: endemic in eastern Africa, Asia, Latin America, and temperate climate zones
- P. ovale: endemic in West Africa
- P. malariae: rarer, endemic in tropical and sub-tropical regions
- P. knowlesi: rarer, endemic in Borneo and Southeast Asia
Of the four, the first is the most common and the main culprit in deaths caused by the disease. Typically, P. vivax, P. ovale and P. malariae do not damage vital organs, so death fatalities tend to be rarer.
TRANSMISSION
Malaria is transmitted to humans by the bites of infected female mosquitos of the Anopheles genus.
Out of the 430 subspecies of Anopheles, approximately 40 are capable of carrying and transmitting the malaria parasite, and are generally distributed in tropical and sub-tropical regions. The main vectors of malaria are the Anopheles Funestus and Anopheles Gambiae mosquitoes.
The mosquito is a heterothermic insect, which means it can only survive in temperatures above 15-18°C, with a high humidity count. The female mosquito feeds on blood to produce and nourish their eggs. They are predominantly active at dusk and at night.
The female mosquito ingests the gametocytes of the parasite when feeding on the blood of an infected person, even if the individual has no symptoms of malaria. Plasmodium gametocytes evolve into sporozoites inside the mosquito; maturation can take a few days or weeks, depending on the climate and species. The sporozoites migrate into the salivary glands of the mosquito, where they are transmitted to humans when the mosquito feeds. This occurs because, before the mosquito can drink the blood, it needs to injects its victim with saliva, which contains an anaesthetic and anticoagulant.
In humans, the parasite continues to mature until it localises in the liver where it invades the hepatocytes (liver cells), maturing into schizont, which lyse (break up the cell, due to rupture of the cell membrane) the blood cells, releasing the plasmodium into the bloodstream in the form of a merozoite.
P.vivax and P. ovale are the only forms that can remain dormant, without causing malaria symptoms. These hypnozoites, can reactivate and cause disease many months later. Merozoite invades red blood cells in the blood stream, where it reproduces, initially developing into a trophozoite, then a schizont. The red blood cell breaks down, releasing merozoites that will go on to invade other red blood cells, perpetuating the cycle. Some parasites differentiate by developing into gametocytes (male and female), which, if ingested can continue to breed inside the mosquito, perpetuating the transmission cycle.
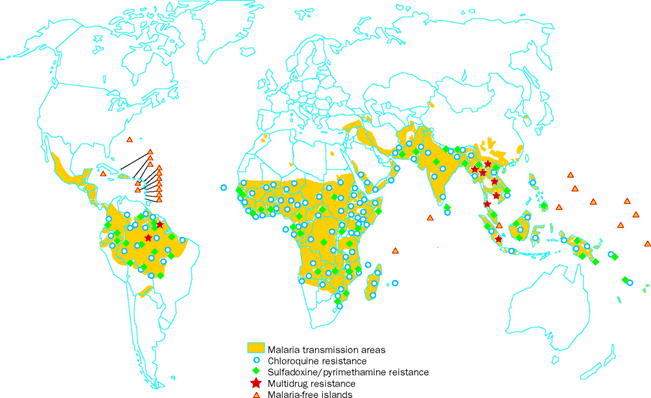
GEOGRAPHICAL DISTRIBUTION
Malaria is mainly prevalent in tropical and sub-tropical regions, where the risk of malaria is very high, due to a number of variables, such as temperature, humidity and rainfall, which are particularly favourable to the proliferation of mosquitoes. Antimalarial prophylaxis is strongly recommended in these areas.
Malaria transmission occurs in areas where the Anopheles mosquito can survive and multiply, and where the parasite is able to complete its growth cycle inside the mosquito itself.
In many of the malaria endemic countries, the spread does not occur in all of the areas, in fact, for example, it is not present in areas with certain characteristics:
- At very high altitudes;
- During the cold/dry season;
- In the desert (excluding oases)
In general, the risk of contracting malaria is higher in regions close to the equator, where it is present all year-round. In particular, sub-Saharan Africa has the highest rate of infection and deaths in the world.
In Southeast Asia, the Middle East, the Pacific, and Central and South America, malaria occurs with varying degrees of endemicity.
SYMPTOMS
The incubation period of malaria prior to symptom onset, usually varies from 7 to 30 days; usually, infection caused by P. falciparum has a shorter incubation period, while P. malaria has a longer incubation period.
It is important to underline that if a traveller has been to a malaria-prone region and requires medical attention for any reason within 12 months from their return, they should inform their health care provider, so that the risk of malaria can be excluded.
The evolution of the disease is classified as uncomplicated, severe (complicated), or recurring malaria.
Symptoms of uncomplicated malaria
The classic symptoms of malaria are characterised by an initial "cold" phase, with symptoms such as shaking chills and feeling cold; a "hot" phase in which there is a rapid rise in fever, headache, nausea; and finally a phase characterised by sweating and a return to normal temperature levels.
Clinical features, such as enlarged spleen and liver, mild jaundice, anaemia, thrombocytopenia, elevated bilirubin, and increased respiratory rate may also occur.
P. falciparum is usually the most severe form of malaria and has the highest risk of developing into severe malaria.
Symptoms of severe (complicated) malaria
Severe malaria occurs when the infection starts to cause severe organ failure or metabolic abnormalities. It is characterised by hyperparasitemia, which is a condition in which more than 5% of the red blood cells are infected with the parasites. The disease can present with severe anaemia, hemoglobinuria, kidney injury, hypoglycemia, metabolic acidosis, blood clotting abnormalities, and respiratory distress syndrome. Severe malaria can also result in cerebral malaria, with seizures, neurological abnormalities, and coma.
Complicated malaria is a medical emergency that requires prompt treatment.
Symptoms of recurring malaria
Infections caused by the plasmodia P. vivax and P. ovale, can be recurring forms of the disease. In fact, both parasites are able to survive in the host organism thanks to their quiescent forms, called hypnozoites, which can reawaken and cause the disease to re-emerge months or years later.
DIAGNOSIS
Early diagnosis is essential to determine effective treatment and good clinical outcome. Suspicion of malaria may arise during clinical examination, either through observation of the symptoms, or from the patient’s medical history (e.g., a recent stay in an endemic area).
Specific diagnosis by means of parasite identification is based on:
- Microscopic search for parasites in a blood sample on a slide;
- Parasite detection in blood using rapid immunoassay tests;
- Search for the parasite's nucleic acids, using PCR
TREATMENT
The choice of elective treatment for malaria is naturally influenced by several factors, such as the type of parasite species involved, the clinical status of the patient, and whether the patient is pregnant or suffers from allergies.
The most frequently used medications include:
- Chloroquine
- Atovaquone-proguanil, trade name: Malarone
- Artemether-lumefantrine, trade name: Coartem
- Mefloquine
- Quinine
- Doxycycline (in combination with quinine)
- Clindamycin (in combination with quinine)
- Tetracycline (in combination with quinine)
- Artesunate
However, the latest World Health Organization (WHO) guidelines on malaria treatment, recommend Artemisinin-based combination therapies (ACTs), as one of the most effective forms of treatment.
PREVENTION
Behavioural prevention
Prevention for malaria starts with correct behavioral prophylaxis.
- Use an effective mosquito repellent
The Centers for Disease Control and Prevention (CDC) recommend repellents with the following active ingredients: DEET (>25%); Picaridin; IR3535; Oil of Lemon Eucalyptus (OLE); Para-menthane-diol; 2- undecanone. - Keep covered
Wear clothes that cover the legs and arms; light-coloured clothing is best. - Check the surrounding environment
Stagnant water is the perfect habitat for mosquitoes to breed. Make sure there is no stagnant water in discarded tyres or industrial containers, swimming pools, storm drains, plant pot saucers, etc. To reduce the risk of transmission, systematic pest control campaigns to fight the Aedes mosquito population appear to be an essential intervention. - Read our in-depth article Don't get stung/bitten!
Malaria chemoprophylaxis
Malaria chemoprophylaxis is especially indicated for people travelling to high risk areas where malaria is endemic.
Accurate assessment of the destination, the time of year and length of stay, the traveller's medical history and condition, and other factors, are essential and can significantly influence the choice of antimalarial prophylaxis.
Currently, the most widely used chemoprophylaxis drugs are:
- Atovaquone-proguanil, trade name: Malarone
- Mefloquine, trade name: Lariam
- Doxycycline, trade name: Bassado, Miraclin
However, it is important to remember that:
- No anti-malarial medication can provide 100 percent protection, consequently, as mentioned previously, travellers should adopt careful personal protective measures, such as: using a good mosquito repellent, wearing appropriate clothing, and sleeping in a mosquito-free environment as much as possible;
- It is essential that tell your travel medicine specialist if you are already taking any of the aforementioned medicines during your pre-trip consultation. This will allow them to assess any possible drug interactions with the prophylactic treatments the traveller will need to take, as well as evaluate any possible allergies/intolerances to the prescribed medication.
Given the complexity of the subject matter and the various clinical, seasonal, geographical, political, and climatic variables, the choice of the appropriate prophylaxis treatment should be made by a qualified travel medicine specialist. With this in mind, below is additional information on the issue of drug resistance.
Drug resistance
Drug resistance is one of the greatest challenges in the fight against malaria.
Resistance to antimalarial drugs has been confirmed only in the case of Plasmodium falciparum and P. vivax. P. falciparum first started to develop resistance to Chloroquine in the 1950s, in Southeast Asia and South America. Today, P. falciparum is endemically resistant to the drug in almost all areas where it exists.
P. falciparum has also developed resistance to sulphadoxine/pyrimethamine, mefloquine (Lariam), halofantrine and quinine. Although resistance to these drugs tends to be much less widespread geographically, in some areas of the world, the impact of multi-drug resistant malaria can be extensive. Resistance to mefloquine is common in parts of Southeast Asia, the Amazon region of South America, and sporadically in Africa.
Chloroquine-resistant P. vivax malaria has been identified in Southeast Asia, Ethiopia, and Madagascar. Vivax malaria parasites, particularly those in Oceania, show greater resistance to this drug than P. vivax isolates in other regions of the world. (CDC; WHO)




