Traveller's diarrhoea
Traveller's diarrhoea is one of the most common travel-related illnesses and can be caused by a variety of factors. Also known as “Montezuma's Revenge”, it affects 30 to 70% of travellers each year.
CAUSES
When travelling, the body is exposed to various stressors to which it needs to adapt, such as tropical climates with high humidity levels, different foods, food storage that is not always adequate, and sanitary conditions that are not always safe.
These factors stress our digestive system, irritating primarily the intestine, which together with the additional risk of exposure to pathogens, all play a key role in the onset of traveller's diarrhoea.
The aetiological agents (causative agents) most commonly involved are bacteria, such as Escherichia coli, Campylobacter jejuni, Shigella, and Salmonella, which cause up to 80% of cases of traveller's diarrhoea. Viruses, such as Rotavirus, Norovirus, Astrovirus, and Hepatitis A virus, cause about 10-15% of diarrhoea cases, while parasitic agents, such as Giardia, Ameba, and Strongyloides, are the third leading cause of all traveller's diarrhoea cases.
TRANSMISSION
Transmission typically occurs via the faecal-oral route: the causative agent is excreted by infected individuals via the faeces and can go on to contaminate the food and drink subsequently consumed by healthy individuals.
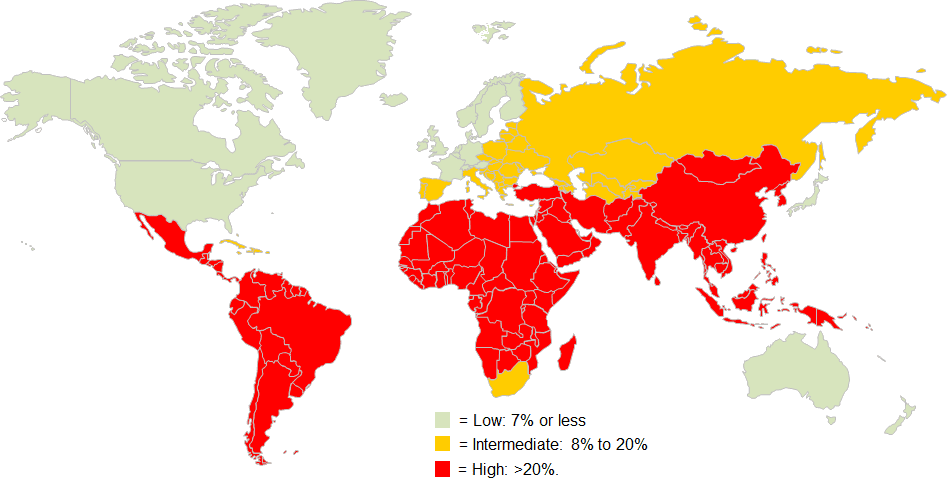
GEOGRAPHICAL DISTRIBUTION
The pathogens that can cause this unpleasant travel companion can be found all over the world, but the destinations with the highest risk are generally in the tropical and sub-tropical regions of the globe, from Asia, the Middle East, and Africa, to Central and South America.
SYMPTOMS
Diarrhoea of bacterial and viral origin usually manifests with the sudden onset of unpleasant symptoms, such as abdominal cramps, unformed or watery stools, fever, vomiting, and general malaise. In cases where symptoms last for several days, or in the event of particularly acute pain, it is advisable to contact a doctor or infectious disease specialist, possibly one who specialises in tropical medicine.
Bacterial pathogens usually cause the first symptoms within a few hours, whereas certain protozoa, such as Giardia or E. histolytica, can have a longer incubation period of approximately 1-2 weeks (except for Cyclospora cayetanensis, which can occur rapidly in high-risk areas).
The clinical course of the illness also differs depending on the pathogen, where observation may be useful for diagnostic purposes. Untreated bacterial diarrhoea can usually last for up to 7 days, while viral diarrhoea has a shorter course, averaging 2-3 days. Whereas, diarrhoea caused by protozoa can persist for weeks or months in the absence of treatment.
DIAGNOSIS
Diagnosis starts from the patient's clinical picture and the characteristics of the travel destination. Once the suspicion of traveller's diarrhoea has been raised, coproculture (the culture of faeces) can be carried out, which allows for the growth and identification of E. Coli strains in the stool. In any case, specific laboratory tests are needed in order to identify the specific aetiological agent.
TREATMENT
Treatment depends on the cause of the illness. Consequently, it is essential to diagnose the pathogen in order to appropriately and effectively treat the disease.
Hydration is the primary intervention to be implemented, often with mineral salt supplementation. The concomitant use of milk enzymes and intestinal disinfectants is also strongly advised.
Special attention should be given to children, the elderly and people with chronic underlying diseases.
In cases of moderate diarrhoea, the CDC recommends treatment with:
- Fluoroquinolones (Ciprofloxacin, Levofloxacin).
- Azithromycin.
- Rifaximin, an antibacterial intestinal disinfectant, which can also be found under the following drug trade names: Normix, Flonorm, Ranbaxy, Rifaximin, and Tixtar.
- Neomycin and Bacitracin are intestinal antibacterial disinfectants. The trade name of the pharmaceutical that contains them is Bimixin.
- Loperamide should never be used on its own but in tandem with antibiotic therapy as it can only treat the symptoms and not the cause. The drug's trade names are: Imodium and Loperamide Angelini. Do not use if you have fever or when blood is present in the stools
PREVENTION
For people travelling in high-risk areas, the CDC recommends several preventive behavioural measures that can help reduce, but never completely eliminate, the risk of traveller's diarrhoea.
- Choose food and beverages carefully
- Eat cooked foots that are still hot. Always wash fruits and vegetables thoroughly;
- Peel fruits and vegetables, whenever possible;
- Avoid meat, raw fish and unpasteurised products;
- Avoid ice in drinks;
- Breastfeeding is advisable when traveling with a baby;
- If you are using formula, mix the powder with hot water that has been heated to a temperature of at least 70°C;
- Always sterilize bottles, baby bottles and pacifiers;
- Beware of water
- In areas where the tap water may not be safe to drink, only use water from sealed, unopened bottles for drinking, preparing food and drinks, ice cubes, cooking, and brushing teeth;
- Beverages made with freshly boiled water, such as tea and coffee, are generally safe to drink;
- Hand hygiene
- Travellers should always wash their hands with soap and water before preparing food and eating, after using the bathroom or changing nappies, before and after caring for someone who is ill, and after contact with animals or their environment;
- If soap and water are not available, use an alcohol-based hand sanitiser (with ≥60% alcohol) and wash hands with soap and water as soon as possible.
No vaccines are not available for most of the agents that cause this illness but there are some very effective vaccines for diseases, such as Cholera, Salmonella, and Hepatitis A.
Source: CDC




