Shigellosis
Shigellosis is an infectious disease, caused by Shigella, a Gram-negative pathogenic bacteria, which is mainly transmitted via the faecal-oral route. Out of the 165 million Shigella cases per year, 1.5 million people die. 98% of these deaths occur in underdeveloped nations and approximately 500,000 were reported in the United States.
Shigella disease causes dysentery, accompanied by vomiting, dehydration, and abdominal pain. Blood and mucus in the stool are good indicators of Shigella infection, but further testing is needed to identify the correct pathogen and administer the appropriate treatment.
CAUSES
Shigella is a member of the Enterobacteriaceae family and can be classified into four serological subgroups:
- S. dysenteriae
- S. flexneri
- S. boydii
- S. sonnei
Although many authors have treated these subgroups of Shigella as distinct taxonomic species, Escherichia coli and Shigella are genetically very similar (80-90%), so much so that nearly all of the Shigella strains could be considered a biotype of E. coli.
Because of their substantial genetic similarity, distinguishing Shigella from E. coli is often a challenge for the microbiology laboratory.
TRANSMISSION
This disease is highly infectious: it only takes 10 to 100 of these organisms to cause the disease. Outbreaks are more frequent in the summer months and occur through faecal-oral transmission, after consuming food or water that has been contaminated with the faeces of an infected individuals.
After 1-4 days the infection, which is non-systemic and enterically invasive, the disease becomes acute leading to destruction of the epithelium of the colon. The damage is irregular and significant, and leads to the main clinical symptom: bloody diarrhoea (which sometimes contains mucus), at times accompanied by abdominal cramps and fever.
Children under the age of 5 are more likely to contract Shigella infection, however people of any age are at risk. Living in shared housing or participating in group activities, all contribute to the spread of bacteria. Shigella outbreaks are most common in day care centres, children’s swimming pools, nursing homes, prisons and military barracks.
People who live or travel in areas without adequate sanitation are more likely to become infected with Shigella.
GEOGRAPHICAL DISTRIBUTION
Shigella still remains a major cause of infant morbidity and mortality. The Global Enteric Multicenter Study (GEMS) recently provided a solid update on the incidence of Shigella compared to other severe forms of diarrhoea, convincingly demonstrating that Shigella was among the leading identified pathogens identified, in the areas under examination (sub-Saharan Africa and Asia).
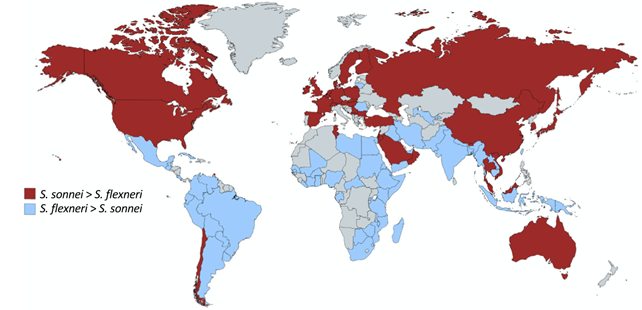
Many studies have reported how the Shigella strains are geographically stratified according to the level of economic development in a given country.
S. flexneri is the main infectious strain in developing regions, while rates of S. sonnei increase in more economically advanced regions.
S. boydii is more commonly restricted to Bangladesh and Southeast Asia, and rarely occurs outside these regions.
S. dysenteriae type 1 (Sd1) occurs sporadically in epidemic settings. A clear example occurred between November 1993 and February 1995, in refugee camps during the civil war in Rwanda, where there were more than 180,000 cases and a significantly high mortality rate.
The worldwide incidence of shigellosis is estimated at 165 million cases. However, the mortality rate has only substantially decreased in the past three decades.
SYMPTOMS
Symptoms of Shigella infection include fever, malaise, watery diarrhoea, abdominal cramps, and muscle aches. The incubation period ranges from 1 to 4 days, and the disease often resolves within 5 to 7 days. After 2-3 days, the volume and frequency of diarrhoea may decrease and can sometimes be followed by blood and mucus in the stool. Some individuals may be asymptomatic but they can still spread the bacteria to others.
Inflammation of the colon is often observed in shigellosis, however this symptom alone is not enough for diagnosis.
Other symptoms include acute renal failure, thrombocytopenia, microangiopathic haemolytic anaemia; the mortality rate is 35%.
Post-reactive arthritis is a complication of Shigella infection that occurs in 2% of cases. It is characterised by joint pain, painful urination, eye irritation, and chronic arthritis that can last a few months to years.
DIAGNOSIS
The clinical diagnosis of shigellosis is complex because it does not differ from other intestinal infections that present with bloody diarrhoea.
The microscopic examination of stool specimens is one of the most effective screening tests for invasive bacterial diarrhoea. However, definitive diagnosis of Shigella-infection can only be made by isolating and identifying the organism from stool samples.
TREATMENT
Antimicrobial therapy has been shown to reduce the duration, transmission and severity of symptoms. First-line treatment for all patients with shigellosis should be fluoroquinolone (such as ciprofloxacin, azithromycin, ceftriaxone).
Fluid loss due to infection is treated orally.
Antidiarrheal treatments should be avoided as they can prolong the duration of the disease.
The choice of treatment is based on the severity of symptoms and is aimed at reducing bacterial spread to avoid the development of more resistant strains.
In fact, some Shigella subtypes are highly resistant to drug treatments (particularly tetracyclines), however, this varies greatly by geographical region.
PREVENTION
Hand hygiene is the cornerstone of prevention, particularly before handling food.
To prevent the spread of Shigella, it is important to implement certain measures, such as:
- Wash hands frequently with soap and water for at least 20 seconds;
- Always help young children to wash their hands thoroughly;
- Dispose of soiled nappies correctly;
- Disinfect baby changing areas after use;
- Do not prepare food for others if you have diarrhoea;
- Keep children with diarrhoea at home and do not take them to child care, playgroup, or school;
- Never drink water from untreated ponds, lakes or pools;
- Avoid sexual intercourse with anyone who has diarrhoea, or people who have recently recovered from diarrhoea;
- Do not go swimming until fully recovered.
Appropriate isolation procedures must be adopted for patients and carriers.
Vaccine
The decrease in the incidence of shigellosis with age suggests the development of natural immunity. This implies that vaccines could also be effective because they elicit such a natural response.
There is currently no licensed Shigella vaccine, but there are a number of vaccines in preclinical or clinical trials, including live attenuated, whole-cell killed, conjugate, and subunit vaccines.
Bibliography
Stephen Bakera and Hao Chung The. Recent insights into Shigella: a major contributor to the global diarrhoeal disease burden. 0951-7375 Copyright 2018 The Author(s). Published by Wolters Kluwer Health, Inc.;
MarkAnderson ,PhilippeJ.Sansonetti andBenoitS.Marteyn. Shigella Diversity and Changing Landscape: Insights for the Twenty-First Century. Frontiers in Cellular and Infection Microbiology April 2016 | Volume 6 | Article 45;
Emily Mattock and Ariel J. Blocker. How Do the Virulence Factors of Shigella Work Together to Cause Disease? Frontiers in Cellular and Infection Microbiology. March 2017 | Volume 7 | Article 64;
Alex N. Frickenstein, Meredith A. Jones, Bahareh Behkam 3 and Lacey R. McNally. Imaging Inflammation and Infection in the Gastrointestinal TractInt. J. Mol. Sci. 2020, 21, 243; doi:10.3390/ijms21010243;
John Dekker and Karen Frank. Salmonella, Shigella, and Yersinia. lin Lab Med. 2015 June; 35(2): 225–246. doi:10.1016/j.cll.2015.02.002 2015 Published by Elsevier Inc;




