Pneumococcus
Pneumococcus (Streptococcus pneumoniae) is a pathogenic bacteria responsible for many, often serious, diseases, including otitis, pneumonia, meningitis, and sepsis. The bacteria frequently affects the most vulnerable, chiefly children under the age of 5 and the elderly population.
Pneumococcus is responsible for most cases of acute otitis in children and is the leading cause of meningitis and pneumonia. As many as 1462 cases of invasive Streptococcus disease were reported in Italy in 2016; while globally, WHO estimates that there are 14.5 million cases of severe disease each year, and the death of children under 5 years of age is approx. 735,000.
Since 2000, the use of a pneumococcal conjugate vaccine in the childhood immunisation program has led to a dramatic decline in invasive pneumococcal disease, in both children and adults. Despite this decrease, the burden of pneumococcal disease in adults over 65 continues to be high.
CAUSES
The disease is caused by the Gram-positive bacteria Streptococcus pneumoniae (also known as pneumococcus), which can survive in both aerobic and anaerobic conditions (i.e., in the presence or absence of oxygen).
Pasteur and Sternberg first isolated S. pneumoniae in saliva, in 1881. Currently, there are varying opinions on the exact number of identified serotypes of S. pneumoniae, which number at least 97.
TRANSMISSION
Transmission occurs through respiratory droplets, produced when someone coughs, sneezes, or simply talks, or through indirect contact with contaminated material.
The severity of pneumococcal diseases has led to multiple studies investigating the mode of transmission of S. pneumoniae. The nasopharynx has been classified as the primary reservoir. This is also due to the fact that the nasopharynx of the hosts can often colonised without producing any symptoms. After colonisation, the spread of the disease will depend on how much the carrier comes into close contact with healthy individuals in the community.
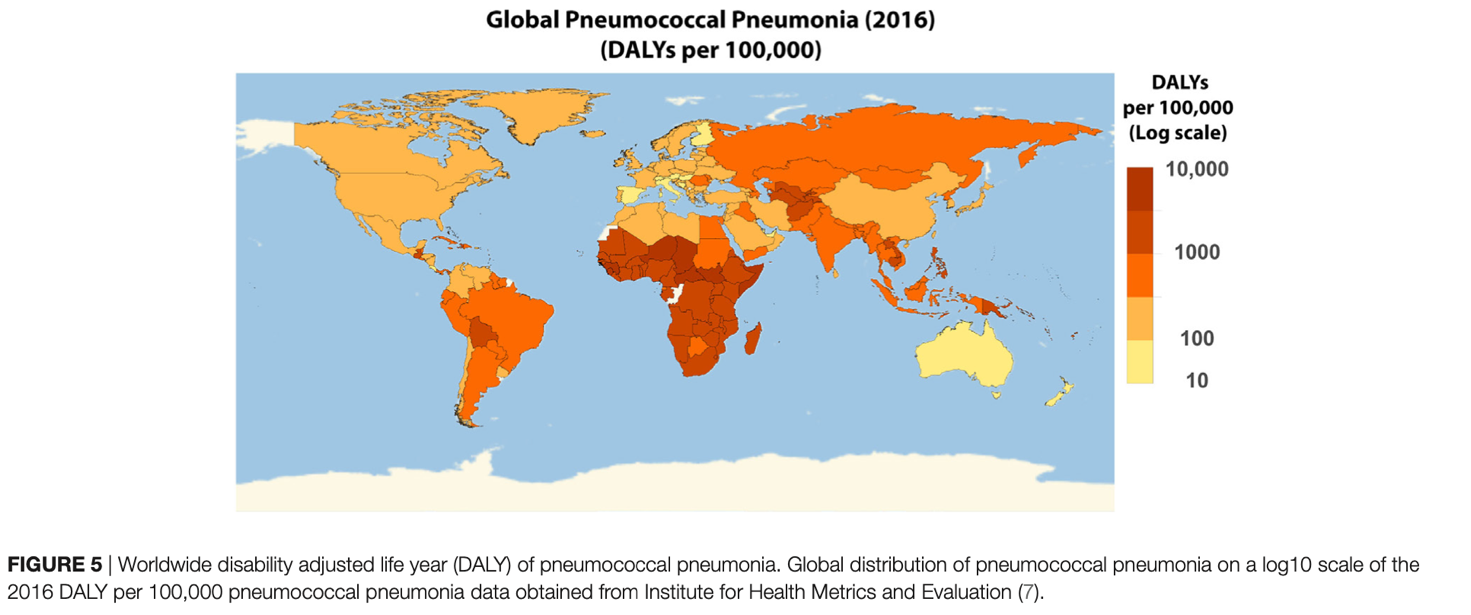
GEOGRAPHICAL DISTRIBUTION
Pneumococcal disease occurs worldwide and is more prevalent in young children, the elderly, and immunocompromised individuals.
S. pneumoniae causes many pneumococcal diseases, including meningitis, bacteraemia, pneumonia, acute otitis media, and sinusitis, and causes approximately 40,000 fatal pneumococcal infections per year in the United States.
SYMPTOMS
After an incubation period that can range from 1 to 3 days (depending on the type of infection), the first symptoms start to appear.
Pneumococcal infections can be classified into two broad categories:
- Invasive infections: affecting vital organs or blood with very serious consequences, for example; meningitis, sepsis, pneumonia, pneumococcal bacteraemia, septic arthritis, and septicaemia.
- Non-invasive infections: these infections are generally easy to resolve without causing permanent damage e.g.; otitis media, sinusitis and conjunctivitis.
The symptoms of a Streptococcus Pneumoniae infection take on different characteristics, depending on the site affected. The most common infections caused by this bacteria are pneumonia, otitis media, and meningitis.
Pneumococcal pneumonia is a form of inflammation of the lungs. The onset of symptoms is typically abrupt with high fever, chills, tachypnoea (increased respiratory rate), cough with rust-coloured sputum, shortness of breath, and chest pain (generally localised to one side), known as lobar pneumonia. In about 40% of cases, excessive fluid forms in the pleural space around the lungs. This leads to pleural effusion, which causes chest pain and difficulty breathing.
Bacterial meningitis is another very serious disease that is caused by pneumococcus. It is an inflammation of the meninges, which are the membranes that protect the brain. On average, symptoms usually occur after an incubation period of 7 days, with abrupt onset of very high fever, headache, convulsions, chills, nuchal rigidity and projectile vomiting.
Pneumococcal meningitis can lead to extremely serious complications, such as, for example, hearing loss (the most common complication), seizures, memory loss, learning disabilities and loss of vision.
Otitis of the middle ear occurs predominantly in childhood, with a case rate of approx. 30%-40%. The condition causes ear pain, accompanied by redness and eversion of the eardrum membrane; pus may also form behind the eardrum.
DIAGNOSIS
Currently, there are several methods for diagnosing pneumococcal disease.
Traditionally, diagnosis starts with a clinical examination. More specifically, in the case of pneumonia, it is based on the results of the objective examination; a chest X-ray can be performed to examine the lungs and monitor inflammation to confirm the presence of infection.
Bacterial cultures and Gram Stain tests on body fluids are important to determine the strain of bacteria and confirm its identity. Due to poor sample yield and quality when conducting cultures, clinicians are currently investigating other means of diagnosing pneumococcal infections. This process also depends on bacterial growth, which can take a long time.
TREATMENT
Treatment of pneumococcal infections relies on antibiotics to reduce the bacterial load and supportive therapies.
Antibiotics works by killing the bacteria or hindering its growth. The first antibiotic created was penicillin, and antibiotics have been widely used ever since. However, improper use of antibiotics can cause bacteria to become resistant. Currently, penicillin-resistant strains have spread worldwide, and pneumococcus is also resistant to other types of antibiotics, i.e. erythromycin, tetracycline and chloramphenicol. In 2013, the CDC estimated that about 30% of pneumococcal cases were due to antibiotic resistance to one or more antibiotics.
PREVENTION
The main form of prevention against pneumococcal infections is vaccination. The two most commonly used vaccines are:
Pneumococcal polysaccharide vaccine 23 (PPSV23) is derived from purified capsular polysaccharides and is routinely administered to adults aged 65 years and older. The vaccine protects against 23 serotypes of S. pneumoniae and is effective in 50-70% of adult cases. PPSV23 provides T-cell-independent immunity and requires a booster every 5 years after the first shot as immunity is only temporary.
The pneumococcal conjugate vaccine (PCV13). This vaccine was developed after noting the low efficacy and scarce immunogenicity of PPSV23 in babies and young children. In the conjugated vaccine, purified polysaccharides are covalently conjugated to a carrier protein. This causes a T-cell-dependent response that provides much stronger and longer lasting mucosal immunity and immunological memory in children.
Currently, children and adults who are at high risk of pneumococcal disease and have pre-existing conditions are being put on a prevention strategy with initial administration of PCV13, followed by PPSV23.
Bibliography & Sitography
Charles Feldman*, Sipho K. Dlamini, Shabir A. Madhi, Susan Meiring, Anne von Gottberg, Janetta C. de Beer, Margreet de Necker, Marthinus P. Stander. The cost-effectiveness of using pneumococcal conjugate vaccine (PCV13) versus pneumococcal polysaccharide vaccine (PPSV23), in South African adults. PLOS ONE | January 29, 2020
Lavida R. K. Brooks1,2 and George I. Mias. Streptococcus pneumoniae’s Virulence and Host Immunity: Aging, Diagnostics, and Prevention. Frontiers in Immunology Review published: 22 June 2018 doi: 10.3389/fimmu.2018.01366
Nadine G. Rouphael and David S. Stephens. Neisseria meningitidis: Biology, Microbiology, and Epidemiology. HHS Public Access, Methods Mol Biol. 2012; 799: 1–20. doi:10.1007/978-1-61779-346-2_1.
Moroni M., Spinello A., Vullo V. Manuale di Malattie Infettive. Edra LSWR, Masson, 2014.
Bartolozzi G. Vaccini e Vaccinazioni, Seconda Edizione. Masson 2015.
Rugarli C., Obiass M., Medicina interna Sistematica, Quinta Edizione. Masson 2015; 1585-1586




