Human Papillomavirus (HPV)
Papilloma virus or HPV (Human Papilloma Virus) is responsible for one of the most prevalent sexually transmitted diseases in the world. An estimated 80% of sexually active women have or have had papilloma virus.
Infections can be asymptomatic, present with warts or be associated with a variety of benign or malignant tumours. Different strains of HPV are responsible for 99.7% of cervical cancers, about 90% of cancers of the anus, 70% of cancers of the vagina, 50% of cancers of the penis, and 26% of cancers of the oropharynx.
The discovery that prevention of high-risk HPV infection can prevent these cancers has prompted the development of HPV vaccines and a worldwide push for prophylactic immunization and timely cervical screening.
HPV-related diseases in Italy have a major economic impact: 291.3 million euros is the average annual direct cost in Italy for secondary prevention and treatment of the top nine diseases and their management (cervical cancer, cervical dysplasia, cancer of the vulva, vagina, anus, penis, and head-neck, genital anal condylomata, and recurrent respiratory papillomatosis).
CAUSES
Papilloma viruses are the etiological agents of warts, papillomas, condylomata, and other benign neoformations and are a genus of viruses consisting of icosahedral capsid formed by 72 capsomeres and resistant to inactivation.
Although more than 205 types of HPV have been isolated, a relatively small number of types (thought to be high-risk HPVs) are responsible for cervical cancer and were later also found to cause most anal, vaginal, oropharyngeal, vulvar, and penile cancers.
Twelve types are known as high-risk types: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59, have been classified as human carcinogens according to the International Agency for Research on Cancer.
Of all high-risk HPV types, HPV 16/18 contribute the most to the development of cervical and oropharyngeal cancers, up to 70% and 90%, respectively. Other countries such as the United States are of particular concern because not only do they have the highest percentage of HPV-induced oropharyngeal cancers, but it is also where the oropharynx has now replaced the cervix as the prevalent site of HPV-related cancers.
|
HPV |
GENOTYPE |
ASSOCIATED DISEASES |
|
High Risk |
16,18,31,33,35,39,45,51,52,56,58,59 |
Cancer: Cervical, anal, vaginal, vulvar, penile and oropharyngeal |
|
Low Risk |
6, 11 |
Warts and recurrent respiratory papillomatosis |
|
Probable carcinogen |
68 |
Cervical cancer |
|
Probable carcinogen |
5, 8 |
|
|
Probable carcinogen |
26,30,34,53,66,67,69,70,73,82,85,97 |
Uncertain |
TRANSMISSION
HPV is a sexually transmitted disease and among infections of this type, the most prevalent on the planet.
The virus is highly contagious and is not stopped even through the use of condoms, which is only partially effective for prevention since infection through non-penetrative intercourse is also possible. Even just a single contact can transmit the virus to a partner, with 60% transmission efficiency each time intercourse takes place.
HPV infections decline sharply with age, probably due to reduced exposure to new partners. This flow is municipality in populations around the world and confirms sexual transmission as the main mode of infection.
Virtually all humans are infected with very different cutaneous HPVs, mainly beta and gamma papilloma viruses, which can act as cofactors for the risk of developing skin cancer in certain human populations.
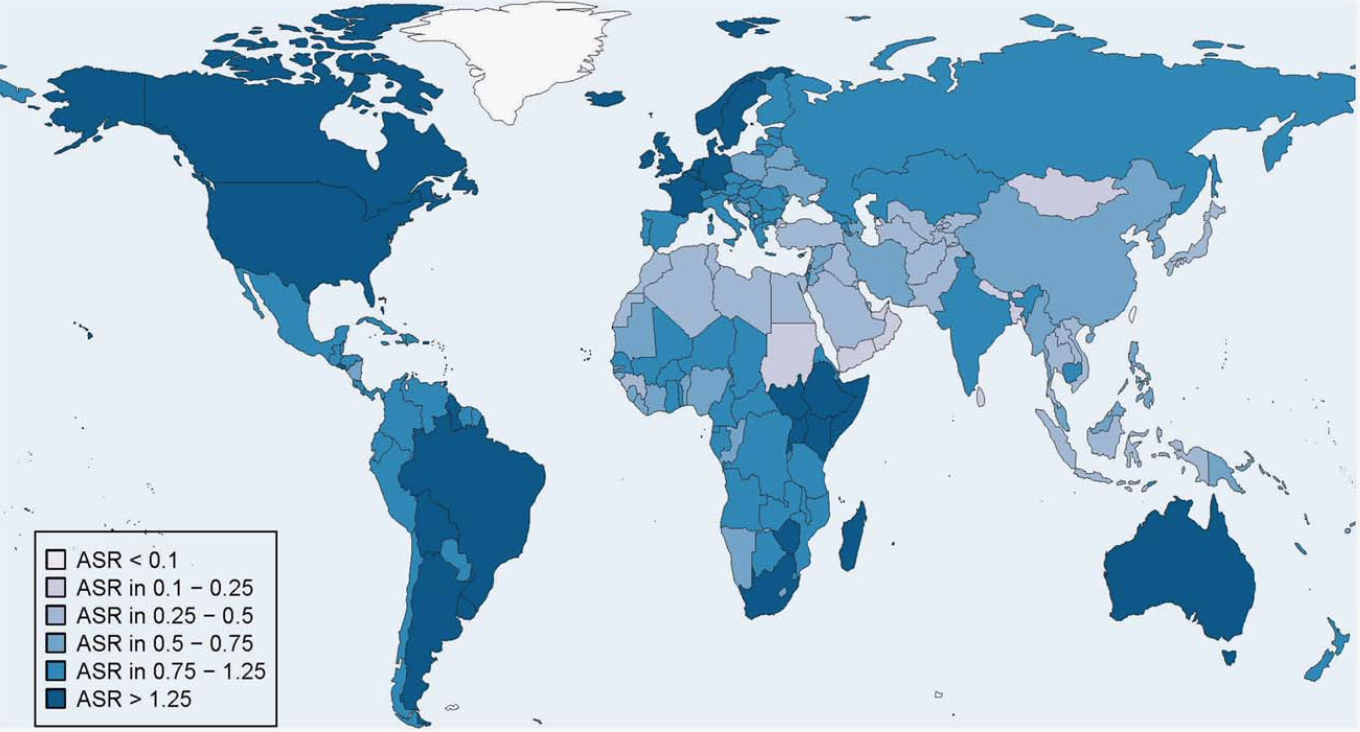
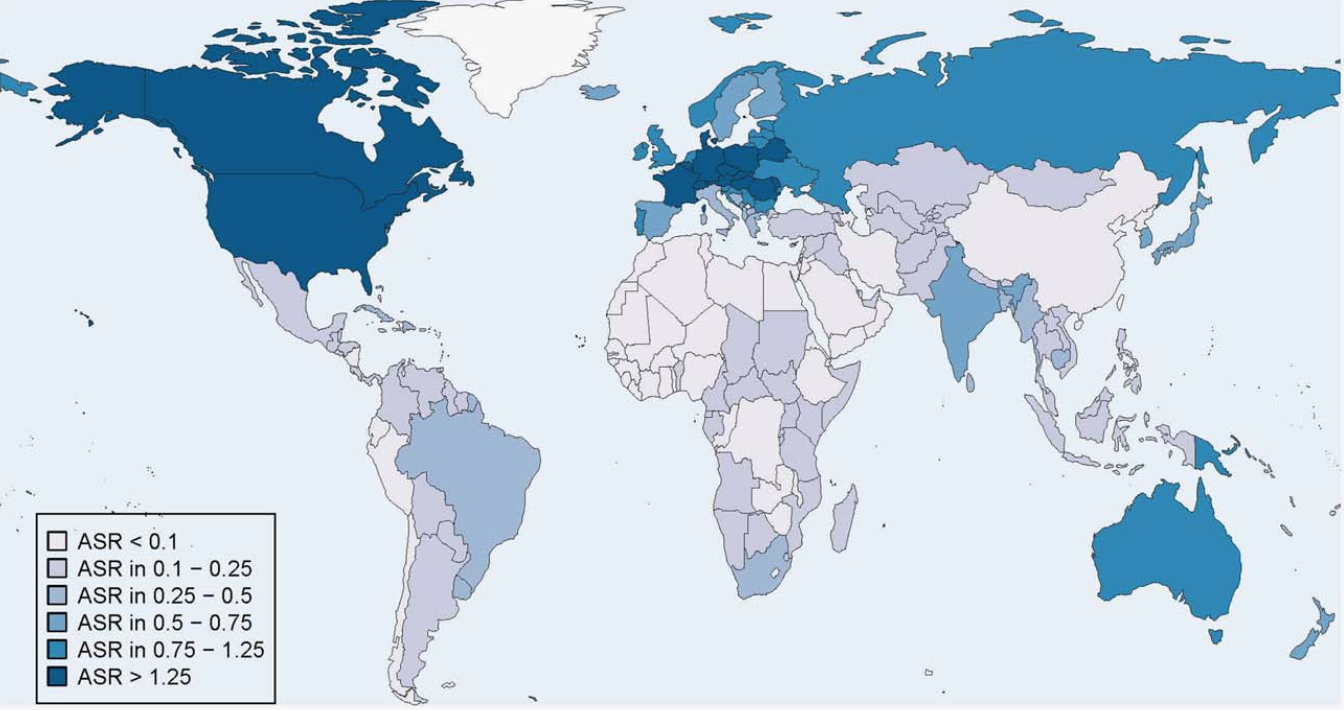
GEOGRAPHICAL DISTRIBUTION
HPV infection is endemic worldwide, and is very common in the population (both female and male): up to 80% of sexually active women come into contact with HPV during their lifetime, with higher prevalence for young women up to 25 years of age. However, the prevalence of the virus is higher in males than in females, and 50% of genital warts are in males. In addition, the diagnosis of tumours in males usually occurs at an advanced stage of carcinoma, which is more difficult to treat.
In China, for example, cervical cancer caused by HPV is the most common type of cancer in the female genital system. It ranks as the eighth most frequent cancer among women in China and is the second most common cancer in women aged 15-44 years.
However, the introduction of the HPV vaccine in many countries has led to major reductions in rates of specific human papilloma virus infection.
Relatively little is known about the natural history of oral HPV infection, but it is likely that subclinical oral HPV infection that persists for decades precedes the development of head and neck cancer caused by HPV.
The reported prevalence of oral HPV infection from individual studies is highly variable because it is influenced by the sampling technique and study population. Oral infection is rare and differs significantly by sex, with a significantly higher prevalence observed in men.
The largest population-based study conducted in the United States (conducted as part of the National Health and Nutrition Examination Survey) reported an oral HPV prevalence of 6.9%, with a significant difference among men.
A high number of lifetime sexual partners, smoking cigarettes and advanced age increase the acquisition of oral HPV infections. Among healthy individuals, the oral prevalence of HPV16 is low (1.3-1.6%) and is consistently lower than what is typically observed in the anogenital region.
SYMPTOMS
Clinical manifestations depend on the type of virus and the site of the lesion. Common warts mainly present on the hands as flesh-colored, hyperkeratotic growths.
Plantar warts can sometimes be painful. When the small thermal vessels bleed, black dots appear on the wart. Flat warts are most common among children and occur on the face, neck, chest, and flexor surfaces of the forearms and legs.
Ano-genital warts occur on the skin and mucosal surface of the external genitalia and perianal areas: they may appear as condylomata acuminata. In men they are most often located on the penis, scrotum, and perianal area: lesions are often localized on the urethral meatus and may later extend.
In women, warts appear first at the posterior fourchette and adjacent part of the labia. They can spread to other parts of the vulva and commonly affect the vagina and cervix. The finding of external lesions suggests the presence of internal lesions, although internal lesions may also be present without external lesions, particularly among women.
DIAGNOSIS
It is essential for diagnosis that women undergo routine periodic examinations through gynaecological prevention programs. In fact, through the evaluation of cytological or histological changes, obtained by Pap Test or other biopsies, the diagnosis of HPV infection can be made.
Among men, HPV prevalence is highest in the penis and lowest in the urethra. Among women, HPV prevalence is highest at the cervix and vagina and lowest at the vulvar epithelium.
Screening is therefore very important for follow-up and early diagnosis.
In addition, further investigations are useful, such as colposcopy, anoscopy and laryngoscopy in the event of tumours affecting the throat,.
TREATMENT
Treatment of papilloma virus infections is based on outcome care.
The decision for initiating therapy must be made based on the knowledge that currently available treatment methods are not fully effective.
It should also be noted that many warts disappear spontaneously. The aim of treatment is to eliminate the lesions rather than to eliminate the virus.
External lesions are removed by cryotherapy, which consists of burning with cold Liquid Nitrogen, laser therapy, diathermocoagulation or hot burning, or surgical excision.
Local treatment of active substances with immunomodulatory effects like Epigallocatechin or cytotoxic effects like Podophylline is also used.
The treatment of condylomata is definitely time-consuming, and even if the lesions are taken away, the virus can remain in the cells and cause new lesions in the future.
Thus, there is a tendency to supplement local therapy with drugs based on systemic targeted phytotherapy active ingredients such as Ellagic Acid complexes with Acetogenine or pure Graviola extract or dextrorotatory and levororotatory methionine with combined zinc.
PREVENTION
Prevention is based on preventive vaccination. The vaccine is available in Italy for prevention of the HPV strains that generally cause precancerous genital lesions of the cervix, vulva, and vagina and invasive lesions of the anus.
As of late 2016, the nonovalent vaccine (Gardasil 9) is the only one available and routine vaccination is recommended at age 11 or 12. This vaccine protects against five other high-risk HPVs (HPV 31/33/45/52/58) not covered by previously developed bivalent or quadrivalent vaccines. The vaccine has been shown to be highly immunogenic, with the potential to prevent an additional 18.3-20% of cervical cancers.
It should be remembered that vaccination is not a substitute for screening because the papilloma virus vaccine cannot be 100% effective and does not result in protection against every viral type.
Secondary prevention, on the other hand, is implemented through early detection of carcinoma precursors by the Pap-test and HPV-test. Performing a Pap test every 3-5 years has been shown in women to reduce the risk of developing invasive cervical cancer by at least 70%.
Bibliography & Sitography
Virgin, H.W.; Wherry, E.J.; Ahmed, R. Redefining chronic viral infection. Cell 2009, 138, 30–50.
ClarkeMA,WentzensenN, MirabelloL,etal. Human papilloma virus DNA methylationasa potential biomarker for cervical cancer. Cancer Epidemiol Biomarkers Prev 2012 Dec;21(12):2125e37.
Verlaat W, Snijders PJF, Novianti PW, et al. Genome-wide DNA methylation profiling reveals methylation markers associated with 3q gain for detection of cervical precancer and cancer. Clin Cancer Res 2017;23(14):3813e22.
Saraiya M, Unger ER, Thompson TD, Lynch CF, Hernandez BY, Lyu CW, Steinau M, Watson M, Wilkinson EJ, Hopenhayn C, Copeland G, Coz- en W, Peters ES, Huang Y, Saber MS, Altekruse S and Goodman MT; HPV Typing of Cancers Workgroup. US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. J Natl Cancer Inst 2015; 107: djv086.
Berman TA and Schiller JT. Human papillomavi- rus in cervical cancer and oropharyngeal can- cer: one cause, two diseases. Cancer 2017; 123: 2219-2229.
Ariel Yusupov, Daniel Popovsky, Lyaba Mahmood, Andrew S Kim, Alex E Akman, Hang Yuan. The nonavalent vaccine: a review of high-risk HPVs and a plea to the CDC. Am J Stem Cells 2019;8(3):52-64 Published December 30, 2019.
Catherine de Martel , Martyn Plummer, Jerome Vignat and Silvia Franceschi. Worldwide burden of cancer attributable to HPV by site, country and HPV type. International Journal of Cancer 141, 664–670 (2017).
Aleyo Chabeda, Romana J.R. Yanez, Renate Lamprecht, Ann E. Meyers, Edward P. Rybicki, Inga I. Hitzeroth. Therapeutic vaccines for high-risk HPV-associated diseases. Papilloma virus Research 5 (2018) 46–58.
Beatriz Serrano, María Brotons, Francesc Xavier Bosch, Laia Bruni. Epidemiology and burden of HPV-related disease. Best Practice & Research Clinical Obstetrics and Gynaecology 47 (2018);
Dingyun You, Liyuan Han, Lian Li, Jingcen Hu, Gregory D. Zimet , Haridah Alia , Mahmoud Danaee, Le Cai, Fangfang Zeng and Li Ping Wong. Human Papilloma virus (HPV) Vaccine Uptake and the Willingness to Receive the HPV Vaccination among Female College Students in China:A Multicenter Study. Vaccines 2020, 8, 31;
Samuel Alizon , Carmen Lía Murall and Ignacio G. Bravo. Why Human Papilloma Virus Acute Infections Matter. Viruses 2017, 9, 293;
zur Hausen H. Papillomaviruses causing cancer: evasion from host-cell control in early events in carcinogenesis. J Natl Cancer Inst. 92: 690-698, 2000;
de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H. Classification of papillomaviruses. Virology 324:17-27, 2004;
Van Ranst M, Kaplan JB, Burk RD.. Phylogenetic classification of human papillomaviruses: correlation with clinical manifestations. J Gen Virol 73:2653-2660, 1992;
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, Snijders PJ, Meijer CJ; International Agency for Research on Cancer Multicenter Cervical Cancer Study Group. 2003. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 348:518-527, 2003;
Ferlay J, Bray F, Pisani P, Parkin DM, GLOBCAN 2002: cancer incidence, mortalità and prevalence worldwide IARC CancerBase No 5, version 2.0. Lyon: IARC Press, 2004;
Kulasingam SL, Hughes JP, Kiviat NB et al.. Evaluation of human papilloma virus testing in primary screening for cervical abnormalities: comparison of sensitivity, specificity, and frequency of referral. JAMA. 288:1749-1757, 2002;
Winer RL, Hughes JP, Qinghua F et al. Condom use and the Risk of genital Human Papilloma virus Infection in Young Women. N Engl J Med 354;25:2645-2654, 2006;
Tornesello ML, Duraturo ML, Botti G, Greggi S, Piccoli R, De Palo G, Montella M, Buonaguro L, Buonaguro FM. And tha italian working group. Prevalence of Alpha Papilloma virus Genotypes in Cervical Squamous Intraepithelial Lesions and Invasive Cervical Carcinoma in the Italian Population. J Med Virol 78:1663-1672, 2006.
Tornesello ML, Duraturo ML, Buonaguro L, Vallefuoco G, Piccoli R, Palmieri S, Buonaguro FM.. Prevalence of human papilloma virus genotypes and their variants in high risk West Africa women immigrants in South Italy. Infect Agent and Cancer 2:1, 2007
Ariel Yusupov, Daniel Popovsky, Lyaba Mahmood, Andrew S Kim, Alex E Akman, Hang Yuan. The nonavalent vaccine: a review of high-risk HPVs and a plea to the CDC. Review Article Am J Stem Cells 2019;8(3):52-64 www.AJSC.us /ISSN:2160-4150/AJSC0100972
Bartolozzi G. Vaccini e Vaccinazioni, Seconda Edizione. Masson 2005.
Baio et al, PLOS ONE 2012; 7 (Issue 11): e49699
Rugarli C., Obiass M., Medicina interna Sistematica, Quinta Edizione. Masson 2015; 1585-1586
Epicentro, il portale dell’epidemiologia per la sanità pubblica: www.epicentro.iss.it
Istituto Superiore di Sanità: www.iss.it
Ministero della Salute: www.salute.gov.it




