Hansen's disease (Leprosy)
Hansen's Disease, better known as Leprosy, is a disease that has accompanied humans since ancient times. Even then, the civilisations of China, Egypt and India considered it an irrepressible, disfiguring and contagious disease. Long considered a hereditarily transmitted disease, the bacteria that causes leprosy was identified in 1873, by Gerhard-Henrik Armauer Hansen, a Norwegian scientist who gave the disease its name.
Despite the discovery of its main etiological factor, Mycobacterium leprae, and advances in every sphere of medical science, the disease continues to be a global public health challenge, especially in underdeveloped and developing countries.
CAUSES
Leprosy is a chronic infection that primarily affects the skin and peripheral nerves. It is caused by Mycobacterium leprae, one of the last bacterial species of medical interest that cannot be cultured in vitro.
It belongs to the Mycobacterium genus of the family Mycobacteriaceae, and is a rod-shaped bacillus that appears immobile under microscopic analysis. It is a microaerophilic, slow-growing bacterium that ideally develops at temperatures between 30° and 35°C. In highly infected tissues, the bacilli join together to form clusters that can number in the hundreds.
A new species of mycobacteria, known as M. lepromatosis, isolated from two deceased patients infected with disseminated lepromatous leprosy, was also identified in 2008. This type of leprosy was first described in 1852, in Mexico, by the scholars Lucio and Alvarado and is named Lucio's Phenomenon after the former.
Whole-genome sequencing of the M. lepromatosis species, conducted during the 2008 study, revealed that M. leprae and M. lepromatosis are quite similar in phylogenetic terms. In fact, they both have the same ancestor and separated over 13.9 million years ago.
TRANSMISSION
The exact mechanisms of leprosy transmission are still unknown.
Leprosy is known to spread through contact between infected patients and healthy individuals, and affects people in all age groups. Several transmission hypotheses have been proposed in medical literature: transmission by the respiratory route, particularly the upper tract, or transmission via insects.
Humans are the main reservoir of infection, but even so, infection has been reported among African monkeys and armadillos in Louisiana.
GEOGRAPHICAL DISTRIBUTION
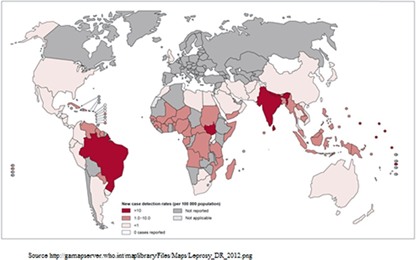
Leprosy is endemically ubiquitous in tropical countries, particularly in underdeveloped and developing countries, with over 200,000 new cases reported each year. A considerable number of cases occur in Southeast Asia, America, Africa, the Eastern Pacific, and Western Mediterranean.
The highest number of reported cases come from Brazil, Indonesia and India, representing over 60% of all new cases.
The epidemiology of leprosy is difficult to understand due to the constant changes to its definition, the lengthy incubation period, and changes in control measures that cause delays in case detection.
SYMPTOMS
The various presentations of the disease can be correlated to the patient's immune response, the infectious load, and late diagnosis.
Leprosy mainly affects the skin and peripheral nerves. Skin lesions are usually the first visible sign, which is why it is considered a dermatological disease. These lesions usually present in the form of macules, hypopigmented or erythematous papules, but also nodules and plaques, that are either the same colour as the skin or slightly red.
In turn, secondary infections due to traumas caused by sensory loss, lead to tissue loss. In fact, the bones and cartilage are absorbed by the infection, causing shortening and deformation.
The subsequent neurological damage can lead to loss of sensation in the skin lesions, hands, or feet. Patients may complain of limb or facial pain, or a numb, pins and needles-type sensation, like "ants running under their skin”, in the affected areas.
Although the tissue damage is triggered by the infiltration of the bacteria, is largely due to the patient’s immune response.
Left untreated, leprosy can progress, causing permanent damage to the skin, nerves, eyes and limbs.
DIAGNOSIS
Early diagnosis of the lesion is crucial for the timely and correct implementation of treatment. This helps prevent the sequelae of the disease, which can lead to considerable physical disabilities and have an immeasurable impact on the individual's social and personal life, which is further aggravated by the stigma associated with the disease.
The diagnosis of leprosy in a patient who has yet to complete a full course of treatment is established when they present with at least one of three basic symptoms:
- Light-coloured or reddish skin patches with localised loss of sensation;
- a thickened or enlarged peripheral nerve, associated with loss of sensation and/or weakness of the muscles affected by that nerve;
- Evidence of acid-fast bacilli in a slit skin smear test.
Depending on the number of lesions, WHO classifies leprosy as follows:
- Multibacillary disease, when the affected individual has more than 5 skin lesions or more than 1 nerve involvement or positive skin smear from any site.
- Paucibacillary disease, diagnosed when there are fewer skin lesions or no nerve involvement, or if there is a single nerve involvement with a negative skin smears from all sites.
This classification is therapeutically useful because paucibacillary cases are treated for 6 months, while multibacillary cases are treated for 12 months using a variety of treatment regimens.
Several other classifications include different criteria, such as clinical, immunological, and histopathological aspects. For example, the Ridley-Jopling classification of leprosy, created in 1966, is based on clinical features, and the histopathological and bacteriological analytical index, which classifies leprosy into five groups:
- Tuberculoid (TT)
- Borderline tuberculoid (BT)
- Mid-borderline (BB)
- Borderline Lepromatous (BL)
- Polar Lepromatous (LL)
The Indian scenario adds another variant, which is a purely neurotic type, characterised only by nerve thickening, sensation impairment with no skin lesions, which can be confirmed by nerve biopsy.
The diagnosis is further reinforced by histopathological examination of the skin biopsy. This indicates that once a full course of medication has been completed, the patient is "cured" and is no longer considered a case of leprosy.
TREATMENT
Multiple drug therapy has revolutionised the duration of treatment, reducing it to a short fixed period. Since 1982, multidrug therapy (dapsone, rifampicin, with or without clofazimine) has been recommended as the standard treatment of leprosy, with a duration of:
- 6 months for patients with paucibacillary leprosy
- 12 months for patients with multibacillary leprosy.
Worldwide use of leprosy drugs began in the 1980s, and their free access since 1995 has contributed to the dramatic decline in the number of new patients.
However, it must be underlined that the disease can recur even after pharmacological treatment. This can be due to insufficient treatment, drug resistance, persistence, or a new infection.
PREVENTION
Despite many efforts to develop a universal active vaccine using DNA techniques, no specific and effective solution against leprosy is available. The BCG (Bacillus Calmette-Guérin) tuberculosis vaccine provides some protection against leprosy, but it is not commonly used to prevent infection.
Although the risk of contracting leprosy is currently low, the best way to prevent the disease is to avoid close physical contact with untreated, infected people.
Bibliography:
Gargi Sarode, Sachin Sarode, PhDa, Rahul Anand, Shankargouda Patil, Mohammed Jafer, Hosam Baeshen, Kamran Habib Awan. Epidemiological aspects of leprosy. December 2, 2019;15:14; 0011-5029 2019 Elsevier.
W.Alemu Belachew, B. Naafs. Position statement: LEPROSY: Diagnosis, treatment and follow-up. European Academy of Dermatology and Venereology. JEADV 2019.
Raissa Gonçalves Couto Dal Secco · Katlein França Massimo Fioranelli · Maria Grazia Roccia. A synopsis of the history of Hansen’s disease. Wien Med Wochenschr. DOI 10.1007/s10354-017-0590-2. 8 April 2017 / Accepted: 17 July 2017. Springer-Verlag.
F. Reibel, E. Cambau, A. Aubry. Update on the epidemiology, diagnosis, and treatment of leprosy La lèpre : actualités épidémiologiques, diagnostiques et thérapeutiques. Médecine et maladies infectieuses. 0399-077X/ 2015 Elsevier Masson SAS.




